Here is a sample that showcases why we are one of the world’s leading academic writing firms. This assignment was created by one of our expert academic writers and demonstrated the highest academic quality. Place your order today to achieve academic greatness.
As a nurse, I must provide patients with safe, compassionate, and devoted treatment according to their individual needs. Besides providing care, it is also essential to ensure that documents are accurately updated to avoid document and treatment errors. However, the documentation helps communicate the superiority of the care clinics provide to all their patients.
Documentation also helps mitigate the probability of risks and the likelihood of malpractice (Scp-health, 2016). This reflection is based on two patients’ documentation errors mixed up while documenting the patient’s details. This reflection utilizes the model of reflection by Rolfe et al. (2010) model. This model is selected as it focuses on the health practitioners’ success and skills rather than favouring self-refection by seasoned professionals.
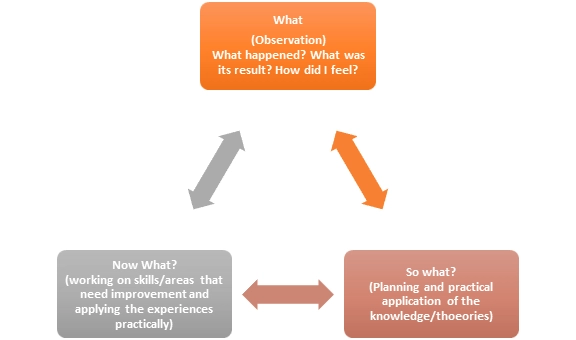
The Rolfe et al. (2010) model, initially published in 2001, begins by asking the same three questions, in line with the Borton (1970) model: What? And so, what? And what now? However, Rolfe et al. (2010) incorporated a higher degree of comprehension into the model, with more information on the questions to be answered and implementing it to improve its accuracy (Skinner and Mitchell, 2016).
After the community placement under my supervisor’s supervision, I got an opportunity to learn various aspects of nursing responsibilities, including patient-centred care, trust-building, and maintaining accurate documentation. According to NMC (2018), professional development prospects keep nurses informed of evidence-based practices and improve their practice.
Whether I was an inexperienced student nurse, I had the excellent opportunity to learn by managing the patients and their records practically. During the reflection, I realized that the student and professional nurses are responsible for patient care (Lachman, 2017). However, the duty of care is not part of the professional code of ethics. Still, it is delegated to all nurses to professionally manage patient care by meeting all patient specifications (Dowie, 2017).
One day I was entering the documentation of my patients as usual. My supervisor instructed me to also document for her patients. I followed her instructions and worked on the patient’s documentation. When I was almost done, I realised that I got two patients’ documentations mixed up. I’ve been working on many patient’s documents since morning, and I realised that I had to rewrite it and was already running late.
Although I was trying to achieve the documents’ accuracy, I was also in a hurry to finish the work on time. I felt irresponsible in terms of managing the documents accurately at the moment. However, I also felt grateful that I could identify the errors before submitting them to the supervisor. It would otherwise have resulted in many other significant negative consequences such as wrong patient treatment, misleading information, and trust issues between patients and health practitioners.
I must address the following concerns while handling the patient’s documentation.
A nurse should handle risk assessment, prepare and provide the patient with high-standard care and treatment according to organizational dimensions of care. As a nurse, my duty will be to guarantee that my patient is provided with evidence-based treatment (Ellis, P., 2019). After I mixed up two patient’s documents, I realised that due to this error, it is more likely that a health practitioner or doctor could face problems identifying each patient’s case history and provide appropriate treatment.
To avoid misleading information and treatment errors, I should be more conscious about handling documents in the future. I discussed this issue with my supervisor to understand how she manages to maintain her documents accurately. However, she listened to me carefully, appreciated my honesty, and taught me the importance of trust and evidence-based practice in nursing.
Gaining the patient’s trust was another topic of concern. Due to conflicting data, there could be a problem of trust between the patient and the nurses. Trust is the cornerstone of safe and successful care and part of patient-centred treatment and the ethical deontology concept (Birkhauer et al., 2017; NMC, 2018).
Besides, trust is also necessary to ensure healthy engagement between healthcare practitioners and patients, bringing positive outcomes (Brennan et al., 2013). What kind of confidence is required in nursing is worth noting (Dyer et al., 2016). Some claim that the patient’s trust and the positive outcome of the treatment/therapies depend on the confidence-sensitivity factor, such as a patient’s perception of nursing skills and treatment satisfaction (Reeves et al., 2017).
My supervisors instructed me to rewrite those documents again efficiently. She also advised me to stay calm, attentive while handling documents. She also gave me some time management and documents organising tips to avoid stress-free work. She also suggested cross-checking the documents before submitting them.
Being more productive and maintaining a professional image in front of the supervisor and the workplace is essential. Meditation is an effective technique to reduce and handle work stress and be attentive to the patients (Bostock et al., 2019). I incorporated meditation in my regular activities, and it not only helped me improve my mental health and boosted my ability to focus.
Being a health care service provider, the skill of attention to detail should be inherited so that every minute detail of my patients is entered into the system to avoid confusion.
Active listening and self-awareness are also important in nursing to ensure patient-centred care (Haley, B. et al., 2017). I gradually started to pay more attention to nursing’s ethical guidelines that keep me updated and motivated to improve my performance.
I realised that I was facing problems with time management managing. I also recalled that I often felt stressed while managing multiple documents. After this incident, I learned the importance of properly arranging documents and listening to instructions. Per my supervisor’s instructions, I made a work schedule and tried to complete daily tasks as per the specific timing of the task. It helped me manage work stress and helped me accomplish the task more actively and accurately. My positive attitude helps me to overcome this situation.
Professional editors proofread and edit your paper by focusing on:
Per the principle of safe practice, inadequate reporting may directly affect patient care (Eveleigh, 2018). As reliable documents, help colleagues stay updated on the patient’s status and enable patient care and safety to be handled effectively (Andrew and St Aubyn, 2015). Duty of candour further stresses the integrity of health practitioners and their conscientious approach (Shoqirat et al., 2019).
If I would have entered my patient’s documentation first, then worked on my supervisor’s documents, the confusion and error could have easily been avoided. Prioritisation of work is also one strategy that ensures proper utilisation of time and delivers supervisors with qualitative and accurate work (Scp-health, 2016). Consequently, I learned to segregate my work according to the one that should be prioritised at the initial stage and then progress to the other.
Also, I started the practise to carefully review each patient’s medical records to know if anything about his/her case has been wrongly reported. The best way to incorporate this skill is by re-checking the data I have entered and ensuring the patients’ minute details. Through this practice, the mistake of wrong documentation can be easily avoided.
If I notice any errors or false details in any report, I would immediately report the matter to my supervisor. Since faulty reports will adversely affect the patient’s care according to the principle of safe practise. To manage patients’ treatment and safety efficiently, updated documentation is important. A health professional should always cross-check the reports to ensure their accuracy and prevent any risk during treatment (Schwappach et al., 2016; RCN, 2016).
Whether I enter the patients’ details manually or use the computer, I incorporated a habit of cross-checking the facts after completing each document before saving it in the system or submitting it to the supervisor. These small, yet effective habits helped me organise and manage my work efficiently and evoke a sense of responsibility and care.
Furthermore, if I also learned if I ever get the responsibility to handle patient’s lab samples, then it is important to submit the patient’s samples to the laboratory by correctly marking them prevent any errors that can impact care (Rodziewicz, T.L., and Hipskind, J.E., 2020). Gathering a patient’s personal information personally and from his documents to ensure consistency and eliminate mistakes is an effective practise to minimise document errors (Khammarnia et al., 2015).
Sometimes, when I had to deal with the patients’ comprehensive information, I also preferred to seek help from my colleagues to cross-check and organise the documents. As a nurse, this kind of interprofessional assistance and relationship will help me obtain professional advice and support if I experience any trouble handling any patient (Kanaskie, M.L., and Snyder, C., 2018).
Despite a lack of expertise and in-depth knowledge, the document management during the reflection was challenging. When I was given the responsibility of handling the various patient’s documents simultaneously, I felt nervous and worried as I had never done this professional work before. However, while participating in it, I enjoyed my duties.
It boosted my confidence, but I also got the chance to learn about different important steps I can follow if I ever encounter such challenges. During the entire process, I tried to interact compassionately and respectfully with the patient, colleagues, and supervisors that helped me correct my mistakes and identify the solution to my problems.
It is worth mentioning that I failed effective management of the documents initially. On the other hand, I’m glad that I could successfully follow my supervisor’s instructions and overcome the challenges of work management that were the core reason behind the documents’ mishandling. During the improvement process, I realised that making small changes in the daily routine such as meditating, active listening, and discussing the issues with colleagues and supervisors positively changed my professional attitude.
Furthermore, the experiences and knowledge I gained from this reflection will enable me to practise and enhance all the essential nursing skills in my future. This will help me eliminate document errors and better manage the patient’s information. For instance, before this reflection, I was unaware of the importance of evidence-based parctise, trust between the patient and health practioner and active listening to eliminate treatment errors.
Now I have the ability to:
In addition, this reflection has encouraged me to evaluate my abilities and skills and helped me recognize my strengths and weaknesses. All my supervisor’s tips and learning experiences will be useful during my nursing practice.
Andrews, A. and St Aubyn, B. (2015) ‘If it’s not written down; it didn’t happen’. Journal of Community Nursing, 29(5), pp. 20. Available at: https://jcn.co.uk/files/downloads/articles/jcn-v29-is5-08-not-written-down-nothappen.pdf (Accessed: 14 January 2021)
Birkhauer, J., Gaab, Jens., Kossowsky, Joe., Hasler, S., Krummenacher, P., Werner, C. and Gerger, H. (2017) Trust in healthcare professional and health outcome: A meta-analysis. Plos one, 12(2), pp.1-13. doi:10.1371/journal.pone.0170988
Bostock, S., Crosswell, A. D., Prather, A. A., & Steptoe, A. (2019). Mindfulness on-the-go: Effects of a mindfulness meditation app on work stress and well-being. Journal of occupational health psychology, 24(1), 127.
Borton and Rolfe’s Models of Reflexive Practice in Healthcare Contexts. Health and Social Care Chaplaincy, 4(1), 10-19.
Borton, T. (1970) Reach, Touch and Teach, London, Hutchinson.
Brennan, N., Barnes, B., Calnan, M., Corrigan, O., Dieppe, P. and Entwistle, V. (2013) Trust in health care- care provider-patient relationship: A systemic mapping review of the evidence base. International Journal for Quality in Healthcare, 25(6), pp. 682-688. doi: https://doi.org/10.1093/intqhc/mzt063
Dowie, I. (2017) Legal, ethical and professional aspects of duty of care for nurses. Nursing Standard, 32(16-19), pp. 47-52. doi: 10.7748/ns.2017.el0959
Dyer, T.A., Owens, J., and Robinson, P.G. (2016) The acceptability of healthcare: from satisfaction to trust. Community Dental health, 33, pp. 242-251. doi:10.1922/CDH_3902Dyer10
Eveleigh, M. (2018) Safe delegation techniques for practice nurses. Nursing in practice. Available at: https://www.nursinginpractice.com/safe-delegation-techniquespractice-nurses (Accessed: 14 January 2021)
Ellis, P., 2019. Evidence-based practice in nursing. Learning Matters.
Kanaskie, M. L., & Snyder, C. (2018). Nurses and nursing assistants decision-making regarding use of safe patient handling and mobility technology: A qualitative study. Applied Nursing Research, 39, 141-147.
Khammarnia M., Kassan, A. and Eslahi, N. (2015) The Efficacy of patient wristband Bar-code on prevention of medical errors: A meta-analysis study. (Accessed: 20 February)
Haley, B., Heo, S., Wright, P., Barone, C., Rettiganti, M.R. and Anders, M., 2017. Relationships among active listening, self-awareness, empathy, and patient-centered care in associate and baccalaureate degree nursing students. NursingPlus Open, 3, pp.11-16.
Lachman, V.D. (2017) Applying ethics of care to your nursing practice. Medsurg nursing, 12(2), pp. 112-116. Available at: 15 Student No: 0725683 http://home.nwciowa.edu/publicdownload/Nursing%20Department%5CNUR310%5C Applying%20the%20Ethics%20of%20Care%20to%20Your%20Nursing%20Practice. pdf (Accessed: 14 Jan 2021)
Nursing and Midwifery Council (NMC) (2018) The Code: professional standards for practice and behaviour for nurses, midwives and nursing associates. Available at: https://www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/nmc-code.pdf (Accessed 14 January 2021)
Reeves, B., Pelone, F., Harrison, R., Goldman, T. and Zwarentein, M. (2017) Interpersonal collaboration to improve professionals, Cochrane Library. Available at: doi/10.1002/14651858.CD000072 Https://www.cochranelibrary.com/edsr/doi/10.1002/14651858.CD000072 (Accessed: 14 January 2021)
Scp-health. (2016). 4 Reasons Why Medical Record Documentation Is Vital | SCP Health. Retrieved 7 January 2021, from https://www.scp-health.com/providers/blog/think-with-your-ink-4-reasons-why-proper-medical-record-documentation-is-vital#:~:text=Conclusion,maintain%20the%20continuum%20of%20care.
Skinner, M., & Mitchell, D. (2016). “What? So What? Now What?” Applying
Schwappach, D.L.B., Pffeiffer, Y. and Taxis, K. (2016) Medical double-checking procedure in clinical practice: a cross sectional survey of oncology nurses’ experience. British MedicalJjournal, 6(6), pp. 1-10. doi: 10.1136/bmjopen-2016- 011394
Shoqirat, N., Mahasneh, D., Deema, L., Carleen, S. and Khresheh, R. (2019) Nursing documentation of postoperative pain management. Nursing Care Quality, 34(3), pp. 279-284. doi: http://dx.doi.org/10.1097/NCQ.000000000000372
To create a Reflective Report:
1. Identify the topic/task.
2. Reflect on your experiences and observations.
3. Analyze the insights gained.
4. Structure the report (intro, body, conclusion).
5. Use appropriate language and style.
6. Edit and proofread for clarity and coherence.
You May Also Like